In this article, we’ll cover the human microbiome which consists of microbes that are both helpful and potentially harmful and how new research suggests that specific genetic variations can make people susceptible to having an imbalanced gut microbiome.
From digesting and assimilating nutrients to even governing your immune system, the microbiome exerts numerous influential effects on your overall health and well-being.
Although various factors can impact the microorganisms residing in your gut, recent research indicates that certain genetic variations may render individuals more prone to experiencing an unbalanced gut microbiome.
Alterations in the gut microbiota’s composition could heighten your vulnerability to conditions like leaky gut and intestinal dysbiosis, which have the potential to affect digestion, metabolism, immunity and various other aspects of health.
Below, we dive deep into the world of genetics and gut health, exploring how genes can influence the composition of your microbiome, the function of your digestive tract, and even your susceptibility to different gut-related disorders.

How Does Human Genetics Shape The Gut Flora And Microbiome?
[1][2][3]
Your microbiome composition sets you apart from those around you and genetic factors play a role in shaping your gut structure. Nevertheless, species of animals that share closer genetic ties tend to exhibit greater similarities in their gut microbiomes. [4]
For instance, when scientists examine the gut microorganisms across various mammal types, they discovered that, despite variations in age, dietary habits and geographical locations, human gut microbes exhibit greater similarities to one another compared to those of other species. [5]
The composition of the microbiome can be influenced by various factors, both genetic and environmental, including [6]:
• Diet and lifestyle choices which have the biggest impact
• Genetic variations that can influence gut structure, diet preferences, body weight and immune system activity
• Location and travels
• Whether you were born vaginally or through C-section
• History of antibiotic exposures
Scientists determine the extent to which a specific trait can be attributed to genetics through the study of heritability. This can involve assessing the prevalence of the trait among identical twins and observing its recurrence within families. Heritability data aids researchers in comprehending the degree of genetic influence on traits that exhibit variability.
Studies involving twins have revealed that certain patterns in the gut microbiome are partially inherited. Identical twins tend to have more similar gut microbiomes compared to non-identical twins. [7]
Certain genetic variants can impact the types of bacterial strains that establish themselves in your gut. Moreover, these bacterial strains can also predict specific hereditary traits.
In a twin study examining common gut bacteria strains in UK twins, Christensenellaceae bacteria, associated with lower BMI, was identified as the most heritable. [8][9] Additional heritable microbe strains, such as Methanobrevibacter and Blautia, suggest that genetics exert an influence over a wider spectrum of gut microbes. [9]
Certain genes associated with obesity have been linked to the prevalence of particular microbes, including Methanobrevibacter, Christensenellaceae, Blautia, and Akkermansia. [10][11]. Scientists posit that genetic variations can influence the gut microbiome, potentially contributing to elevated body weights. [7]
Certain highly heritable microbes appear to remain consistent over extended durations, making them less susceptible to influences like diet and lifestyle. [6]
Nevertheless, twin studies also indicate alterations in gut composition as time progresses, underscoring the significant role that the environment plays in shaping the microbiome. [12] One could argue that these factors might have an even more substantial impact on the microbiome than genetics!
Certain genes can still influence your gut health through various mechanisms, which we will explore further below. It is important to note that this list is not exhaustive, as researchers continue to uncover additional ways in which our gut bacteria interact with our genes.
Genes That Affect The Gut Flora
MUC2
[13][14][15][16]
The MUC2 gene encodes a protein called mucin-2, which forms part of the mucus barrier between your microbiome and intestinal lining. Some gut bacteria eat this protective lining as fuel. Parts of mucin-2 also provide nutrients like carbon and nitrogen, which helps fuel good bacteria in your gut.
Scientists identified this gene by breeding mice lacking the MUC2 gene. These mice subsequently experienced significant inflammation in their digestive tracts because they no longer possessed a protective mucus lining. This defect led to dysbiosis and disease.
FUT2
[17][18][19][20][21]
The FUT2 gene encodes a protein called fucosyltransferase 2, which helps synthesize molecules in your digestive tract. Specifically, it plays an important role in attaching fructose (sugar) molecules to the mucin proteins discussed above.
Fructose serves as a critical energy source for specific bacteria, aiding them in adhering to the gut lining and evading detection by your immune system.
Certain variations in the FUT2 gene can hinder the colonization of beneficial bacteria in the digestive tract and modify the composition of the gut microbiome. This, in turn, can disrupt the equilibrium between beneficial and harmful microorganisms. Individuals with less functional FUT2 genes often exhibit a lower presence of beneficial bacteria like Bifidobacterium and Bacteroidetes in their gut, leading to an overall less resilient gut microbiome.
LCT
[22][23]
The LCT gene encodes for the enzyme lactase, which helps your body break down lactose sugars found in dairy products.
Genetic variations in the LCT gene are linked to lactose intolerance. Individuals with LCT gene variants may experience diminished lactase activity, leading to the development of lactose intolerance symptoms when they consume dairy products. This can affect how much lactose gut bacteria can ferment.
Fortunately, other studies indicate that dietary adjustments can be beneficial. Incorporating prebiotic galactans, which are present in legumes, can alleviate lactose intolerance symptoms. These molecules have the potential to stimulate the proliferation of beneficial bacteria that aid in lactose digestion while generating fewer instances of gas and other symptoms.
Can Gut Bacteria Be Inherited?
[24][25][26][27][28]
The initial three years of life witness swift alterations in flora composition due to environmental exposures such as dietary choices, antibiotic use, birth method and whether breastfeeding was part of the early upbringing. All of these factors help to shape the flora you have as an adult.
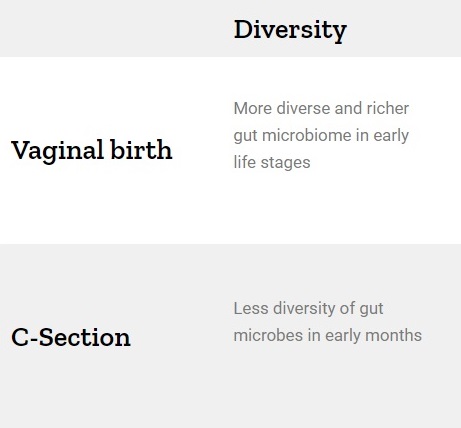
Your gut microbiome is first colonized during birth. And the method in which you were born can have a major impact on its composition.
During vaginal childbirth, it is common for mothers to expel faeces, and for newborns to ingest a mixture of their mother’s faeces and vaginal fluids. In essence, vaginal delivery exposes the baby to the maternal vaginal and gut flora, which forms the initial colonization of the infant’s gut microbiota.
Conversely, if you were delivered via a Cesarean section (C-section), your primary exposure is to skin and environmental bacteria, rather than inheriting them from your mother.
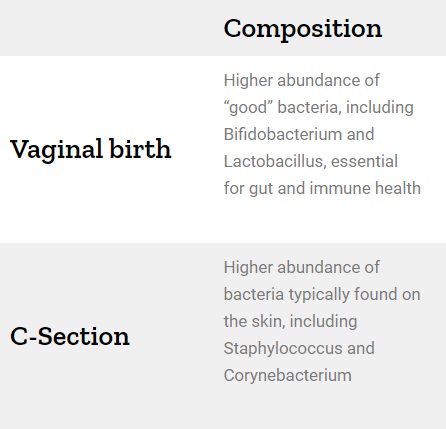
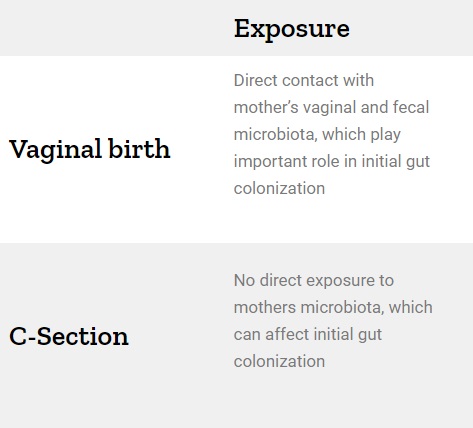
Here are some of the biggest differences:
Diversity
Composition
Exposure
Vaginal birth
More diverse and richer gut microbiome in early life stages
Higher abundance of “good” bacteria, including Bifidobacterium and Lactobacillus, essential for gut and immune health
Direct contact with mother’s vaginal and fecal microbiota, which play important role in initial gut colonization
C-Section
Less diversity of gut microbes in early months
Higher abundance of bacteria typically found on the skin, including Staphylococcus and Corynebacterium
No direct exposure to mothers microbiota, which can affect initial gut colonization
Breast milk provides another avenue for the transmission of microbes from mother to baby. It contains a multitude of beneficial bacteria and prebiotics, which contribute to the development of a healthy gut. It’s worth noting that the precise microbes present in breast milk can differ among mothers.
Close cohabitation with family members also can facilitate the exchange of microbes that eventually find their way into the gut. Families residing together typically exhibit more similar microbiome compositions compared to relatives who live separately. Therefore, gut flora and microbiomes are naturally inherited.
Breast milk provides another avenue for the transmission of microbes from mother to baby. It contains a multitude of beneficial bacteria and prebiotics, which contribute to the development of a healthy gut. It’s worth noting that the precise microbes present in breast milk can differ among mothers.
Close cohabitation with family members also can facilitate the exchange of microbes that eventually find their way into the gut. Families residing together typically exhibit more similar microbiome compositions compared to relatives who live separately. Therefore, gut flora and microbiomes are naturally inherited.
What Affects The Gut Microbiome Beyond Your Genes?

In addition to genetics, numerous other factors can shape the composition of your gut microbiome. Some of the key influencers include:
1) Diet
[29][30][31]
The type of food you eat regularly can directly impact the composition of your microbiome:
• Fiber-rich diets and plant-based foods can promote a diverse and healthy gut microbiome. On the other hand, diets high in processed foods, sugar, and unhealthy fats can negatively impact the gut microbiome.
• Probiotics, the live beneficial bacteria found in fermented foods, also promote gut health. Prebiotics on the other hand, which act as fuel sources for good gut bacteria, can also promote a healthy gut composition.
2) Physical Activity
[31][32][33]
Engaging in physical activity can foster a more robust gut microbiome, encouraging greater microbial diversity and positive alterations in its composition.
Consistent physical activity has been demonstrated to elevate the levels of beneficial bacteria such as Akkermansia and Bacteroides, which are associated with favourable gut health and metabolism. Conversely, a sedentary lifestyle can have adverse effects on the gut, leading to decreased microbial diversity.
3) Sleep
[34][35]
Inadequate or insufficient sleep can likewise exert detrimental effects on the composition of the microbiome. Sleep deprivation can lead to a reduction in the variety of gut microbes and alter the abundance of others.
Certain studies have identified that individuals experiencing poor sleep tend to exhibit elevated levels of harmful gut bacteria like Firmicutes and decreased levels of beneficial bacteria such as Bacteroidetes. Sleep deprivation can also disrupt the metabolism of gut microbes, potentially contributing to an inflamed gut lining.
4) Stress
[36]
Maintaining elevated stress levels, particularly over extended durations, can adversely influence both the composition and functionality of your microbiome.
Stress can lead to alterations in the equilibrium between beneficial and detrimental gut bacteria. Specifically, it tends to reduce the presence of beneficial Lactobacillus and Bifidobacterium while promoting an increase in potentially harmful Clostridium and Escherichia coli.
5) Age
[37][38]
Age significantly influences the configuration of your microbiome, causing variations in diversity and richness over time.
Infants possess a markedly distinct gut flora composition when compared to adults. In the early stages of life, the microbiome is considerably less diverse than that of an adult. Nonetheless, during this period, it undergoes rapid and dynamic changes.
In adults, the microbiome generally maintains stability and equilibrium. However, as individuals age and reach their senior years, we observe further changes, with older adults experiencing decreased microbial diversity and modifications in the abundance of specific bacterial species.
6) Infections & Disease
[39][40]
Numerous infections and illnesses have the potential to disrupt the gut microbiome. Some of these may have genetic factors, as discussed earlier, while others can be associated with autoimmune disorders and gastrointestinal infections.
Certain conditions can lead to dysbiosis, characterized by an overabundance of harmful gut bacteria and a reduction in beneficial ones. Additionally, some conditions can disrupt the immune response in the digestive tract, potentially leading to inflammation and alterations in the microbial composition within the gut.
Viral infections, such as norovirus, can infect cells that line the gut, and cause changes in the gut microbiome. Some of these effects can be short-term, while others can become chronic and this can impact your overall health.
7) Medications
[41]
Exposure to antibiotics can disturb the equilibrium of your gut microbiome by altering the balance of microorganisms within the digestive tract. While these medications are effective at eliminating harmful bacteria that may cause infections, they can also have adverse effects on beneficial bacteria.
Besides antibiotics, other medications such as proton-pump inhibitors and NSAIDs can also affect the gut.
Conclusion
Our understanding of the genetic influence on the gut microbiome is still evolving. While we recognize that genetic factors can affect both the composition and functionality of the gut, there remains much more to discover in this field.
The microbiome is a dynamic ecosystem influenced by genetics, as well as diet and lifestyle. Collectively, these factors can have cascading effects on various bodily processes, potentially exerting both positive and negative impacts on your overall health.
While genetics can provide insights into your susceptibility to dysbiosis and other gut-related conditions, dietary and lifestyle adjustments also play a crucial role in enhancing microbiome diversity and composition.
Here are some actionable steps you can take today to support the health of your gut microbiome:
• Eat a diverse range of fibre-rich foods and fermented foods
• Limit processed and high-sugar foods
• Avoid unnecessary antibiotic and NSAID use
• Manage stress
• Ensure you get enough sleep
• Exercise regularly
• Stay hydrated
• Consider probiotic supplements
By comprehending the significance of your microbiome and your genetic predisposition, you can make informed decisions to promote your gut health. If you’re keen on delving deeper, consider exploring your individual genetic profile and collaborating with a healthcare provider to receive personalized guidance tailored to your specific genetic insights.
References
- Cahana I, Iraqi FA. Impact of host genetics on gut microbiome: Take‐home lessons from human and mouse studies. Animal Model Exp Med. 2020;3(3):229-236. doi:10.1002/ame2.12134
- Bubier JA, Chesler EJ, Weinstock GM. Host genetic control of gut microbiome composition. Mamm Genome. 2021;32(4):263-281. doi:10.1007/s00335-021-09884-2
- Grieneisen L, Dasari M, Gould TJ, et al. Gut microbiome heritability is nearly universal but environmentally contingent. Science. 2021;373(6551):181-186. doi:10.1126/science.aba5483
- Ley RE, Hamady M, Lozupone C, et al. Evolution of mammals and their gut microbes. Science. 2008;320(5883):1647-1651. doi:10.1126/science.1155725
- The Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486(7402):207-214. doi:10.1038/nature11234
- Hall AB, Tolonen AC, Xavier RJ. Human genetic variation and the gut microbiome in disease. Nat Rev Genet. 2017;18(11):690-699. doi:10.1038/nrg.2017.63
- Lim MY, You HJ, Yoon HS, et al. The effect of heritability and host genetics on the gut microbiota and metabolic syndrome. Gut. 2017;66(6):1031-1038. doi:10.1136/gutjnl-2015-311326
- Goodrich JK, Waters JL, Poole AC, et al. Human genetics shape the gut microbiome. Cell. 2014;159(4):789-799. doi:10.1016/j.cell.2014.09.053
- Goodrich JK, Davenport ER, Beaumont M, et al. Genetic determinants of the gut microbiome in UK twins. Cell Host Microbe. 2016;19(5):731-743. doi:10.1016/j.chom.2016.04.017
- Beaumont M, Goodrich JK, Jackson MA, et al. Heritable components of the human fecal microbiome are associated with visceral fat. Genome Biol. 2016;17(1). doi:10.1186/s13059-016-1052-7
- Million M, Angelakis E, Maraninchi M, et al. Correlation between body mass index and gut concentrations of Lactobacillus reuteri, Bifidobacterium animalis, Methanobrevibacter smithii and Escherichia coli. Int J Obes (Lond). 2013;37(11):1460-1466. doi:10.1038/ijo.2013.20
- Xie H, Guo R, Zhong H, et al. Shotgun metagenomics of 250 adult twins reveals genetic and environmental impacts on the gut microbiome. Cell Syst. 2016;3(6):572-584.e3. doi:10.1016/j.cels.2016.10.004
- Boltin D, Perets TT, Vilkin A, Niv Y. Mucin function in inflammatory bowel disease: An update. J Clin Gastroenterol. 2013;47(2):106-111. doi:10.1097/mcg.0b013e3182688e73
- Smith, A.C. and Podolsky, D. K. Colonic mucin glycoproteins in health and disease. Clinics in Gastroenterology. 1986;15(4):815-837. https://www.ncbi.nlm.nih.gov/pubmed/3536210
- Johansson MEV, Phillipson M, Petersson J, Velcich A, Holm L, Hansson GC. The inner of the two Muc2 mucin-dependent mucus layers in colon is devoid of bacteria. Proc Natl Acad Sci U S A. 2008;105(39):15064-15069. doi:10.1073/pnas.0803124105
- Lehrer RI, Lu W. α-Defensins in human innate immunity: Α-Defensins. Immunol Rev. 2012;245(1):84-112. doi:10.1111/j.1600-065x.2011.01082.x
- Kelly RJ, Rouquier S, Giorgi D, Lennon GG, Lowe JB. Sequence and expression of a candidate for the human secretor blood group α(1,2)fucosyltransferase gene (FUT2). J Biol Chem. 1995;270(9):4640-4649. doi:10.1074/jbc.270.9.4640
- Kashyap PC, Marcobal A, Ursell LK, et al. Genetically dictated change in host mucus carbohydrate landscape exerts a diet-dependent effect on the gut microbiota. Proc Natl Acad Sci U S A. 2013;110(42):17059-17064. doi:10.1073/pnas.1306070110
- Tong M, McHardy I, Ruegger P, et al. Reprograming of gut microbiome energy metabolism by the FUT2 Crohn’s disease risk polymorphism. ISME J. 2014;8(11):2193-2206. doi:10.1038/ismej.2014.64
- Frank DN, St. Amand AL, Feldman RA, Boedeker EC, Harpaz N, Pace NR. Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci U S A. 2007;104(34):13780-13785. doi:10.1073/pnas.0706625104
- Tailford LE, Crost EH, Kavanaugh D, Juge N. Mucin glycan foraging in the human gut microbiome. Front Genet. 2015;6. doi:10.3389/fgene.2015.00081
- Bonder MJ, Kurilshikov A, Tigchelaar EF, et al. The effect of host genetics on the gut microbiome. Nat Genet. 2016;48(11):1407-1412. doi:10.1038/ng.3663
- Blekhman R, Goodrich JK, Huang K, et al. Host genetic variation impacts microbiome composition across human body sites. Genome Biol. 2015;16(1). doi:10.1186/s13059-015-0759-1
- Tamburini S, Shen N, Wu HC, Clemente JC. The microbiome in early life: implications for health outcomes. Nat Med. 2016;22(7):713-722. doi:10.1038/nm.4142
- Bennett PR, Brown RG, MacIntyre DA. Vaginal microbiome in preterm rupture of membranes. Obstet Gynecol Clin North Am. 2020;47(4):503-521. doi:10.1016/j.ogc.2020.08.001
- Gupta P, Singh MP, Goyal K. Diversity of vaginal microbiome in pregnancy: Deciphering the obscurity. Front Public Health. 2020;8. doi:10.3389/fpubh.2020.00326
- Ho NT, Li F, Lee-Sarwar KA, et al. Meta-analysis of effects of exclusive breastfeeding on infant gut microbiota across populations. Nat Commun. 2018;9(1). doi:10.1038/s41467-018-06473-x
- Lif Holgerson P, Harnevik L, Hernell O, Tanner ACR, Johansson I. Mode of birth delivery affects oral Microbiota in infants. J Dent Res. 2011;90(10):1183-1188. doi:10.1177/0022034511418973
- Dahl WJ, Rivero Mendoza D, Lambert JM. Diet, nutrients and the microbiome. In: Progress in Molecular Biology and Translational Science. Vol 171. Elsevier; 2020:237-263.
- Zmora N, Suez J, Elinav E. You are what you eat: diet, health and the gut microbiota. Nat Rev Gastroenterol Hepatol. 2019;16(1):35-56. doi:10.1038/s41575-018-0061-2
- Campaniello D, Corbo MR, Sinigaglia M, et al. How diet and physical activity modulate gut Microbiota: Evidence, and perspectives. Nutrients. 2022;14(12):2456. doi:10.3390/nu14122456
- Mohr AE, Jäger R, Carpenter KC, et al. The athletic gut microbiota. J Int Soc Sports Nutr. 2020;17(1). doi:10.1186/s12970-020-00353-w
- Marttinen M, Ala-Jaakkola R, Laitila A, Lehtinen MJ. Gut Microbiota, probiotics and physical performance in athletes and physically active individuals. Nutrients. 2020;12(10):2936. doi:10.3390/nu12102936
- Han M, Yuan S, Zhang J. The interplay between sleep and gut microbiota. Brain Res Bull. 2022;180:131-146. doi:10.1016/j.brainresbull.2021.12.016
- Smith RP, Easson C, Lyle SM, et al. Gut microbiome diversity is associated with sleep physiology in humans. PLoS One. 2019;14(10):e0222394. doi:10.1371/journal.pone.0222394
- Madison A, Kiecolt-Glaser JK. Stress, depression, diet, and the gut microbiota: human–bacteria interactions at the core of psychoneuroimmunology and nutrition. Curr Opin Behav Sci. 2019;28:105-110. doi:10.1016/j.cobeha.2019.01.011
- Badal VD, Vaccariello ED, Murray ER, et al. The gut microbiome, aging, and longevity: A systematic review. Nutrients. 2020;12(12):3759. doi:10.3390/nu12123759
- Conway J, A Duggal N. Ageing of the gut microbiome: Potential influences on immune senescence and inflammageing. Ageing Res Rev. 2021;68(101323):101323. doi:10.1016/j.arr.2021.101323
- González R, Elena SF. The interplay between the host microbiome and pathogenic viral infections. MBio. 2021;12(6). doi:10.1128/mbio.02496-21
- Trakman GL, Fehily S, Basnayake C, et al. Diet and gut microbiome in gastrointestinal disease. J Gastroenterol Hepatol. 2022;37(2):237-245. doi:10.1111/jgh.15728
- Weersma RK, Zhernakova A, Fu J. Interaction between drugs and the gut microbiome. Gut. 2020;69(8):1510-1519. doi:10.1136/gutjnl-2019-320204